As low back pain sufferers already know, it’s very difficult to exercise and train at a high level when you are experiencing low back pain (LBP). Nothing will derail your best laid training plans and routines faster than a severe episode of low back pain. LBP is the most common injury and pain complaint for athletes and non-exercisers alike. It’s estimated to affect nearly 80% of the U.S. population at one time or another, and it’s one of the top reasons for physician visits.
Fortunately, most LBP is mechanical–meaning it’s from a physical or structural cause not related to conditions such as cancer or infections. The problem with this type of LBP is that it usually comes back. People who have had an episode of mechanical LBP are 90% more likely to experience it again.
If you want to train hard and compete at a high level or even just enjoy the weekend’s events, then avoiding LBP is critical. Avoiding the following three most common mistakes can save you from costly medical visits, prescriptions, chiropractic visits, and physical therapy services. More importantly, avoiding injury and LBP insures that you can keep training to your heart’s content!

The 3 Most Common Mistakes:
Sitting too much.
Prolonged sitting (and especially, prolonged sitting on a vibrating surface) is one of the biggest risk factors for LBP. Sitting (slouched in particular) causes excessive strain on the lumbar discs and ligaments. Even if you exercise regularly, many of us still work in an office setting which forces us to sit more than we should. This excessive and prolonged sitting not only impacts our spine, but it also leads to tight hamstrings and hip flexors and generally tends to inhibit proper gluteal muscle function.
Even if you are running, exercising, and training during most days of the week, we all spend too much time sitting. To make this worse, many of us are sitting with chronically poor posture.
- Limit the amount of sitting that you spend at one time. Ideally, move from your sitting position every hour to walk preferably. If you aren’t able to walk, then try to shift your position at least once every twenty minutes. Frequent position changes can help you to avoid LBP. Avoid a long car trip directly before or after a long run, race or event. For destination events, it’s best to arrive at least a day or two early and wait a day prior to returning home.
- Sit with correct posture. Whenever possible, make sure that your knees stay below your hip level and that you are able to maintain your natural lumbar curve. A McKenzie Lumbar Roll is a great tool to help you maintain correct posture.
Poor core training.
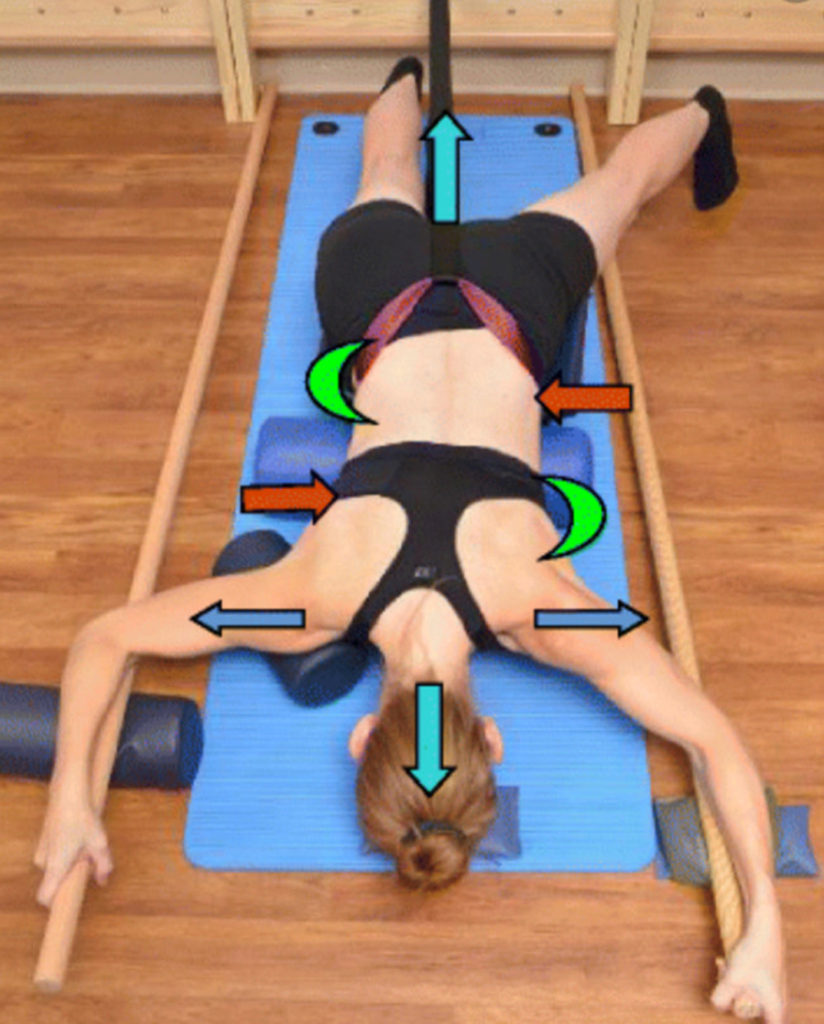
Everyone has heard about the benefits of core training. However, most people aren’t doing it correctly. This isn’t about sit ups or crunches. Proper core strength involves training your abdominal muscles and back extensors to produce a rigid cylinder when exercising and moving. The core muscles are not prime movers, but stabilizers. They must be trained this way. The strength needs to be proportional front to back to insure this rigid cylinder for proper spinal stabilization. In general, most of us don’t spend enough time strengthening a key core muscle in back known as the multifidus (shown below) nor do we spend enough time strengthening the back extensors in general.
The core muscles are part of the body’s natural method of stabilizing the spine. The core muscles, along with intra-abdominal pressure, help to form a round rigid cylinder that is utilized to support the spine. Ligaments and boney articulations are also important in spinal stabilization. Most people don’t realize that the core actually consists of two separate groups of muscles, the inner and outer core muscles, and neither group involve the rectus femoris muscles (the six pack).
- The inner core consists of the muscles of the pelvic floor, the transversus abdominis (TVA), diaphragm, and the multifidus muscles (which span the vertebrae along the back side of the spine as shown above). The TVA wraps all the way around the stomach and attaches to the spine. This is what helps to form the cylinder. When contracted (in conjunction with the pelvic floor and diaphragm), it helps to increase the intra-abdominal pressure to support the spine.
- The other muscles that help to support the spine are known as the outer core. These muscles are responsible for movement of the trunk and spine as well as aiding in stability. The inner core muscles do not actually produce any trunk or spine movement. The outer core muscles consists of the following muscles: lumbar paraspinal muscles; the quadratus lumborm; the internal and external obliques; and the psoas major and minor (hip flexors). Some may also include the glutes (buttocks muscles), hamstrings, and quadriceps as part of the outer core muscles.
Those who work on core strength may not be performing the correct exercises. Performing proper core exercises and particularly, lumbar stabilization exercises are the primary treatment modality for LBP.
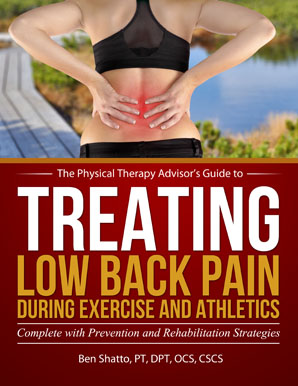
To learn how to effectively exercise and work the core muscles in order to prevent or self-treat LBP, be sure to check out my Treating Low Back Pain (LBP) during Exercise and Athletics Book and Video Package. USE DISCOUNT CODE LBP AT CHECKOUT FOR 15% OFF!
Not performing a proper warm up.
An adequate warm up should always be performed to help minimize the risk of injury and maximize your ability to perform at an optimal level. A proper warm up should include: a cardiovascular warm up; a dynamic warm up; a specific spine warm up; and when indicated, a sport specific warm up.
Cardiovascular Warm Up
To properly prepare the body for activity, the first stage of the warm up is to increase blood flow throughout the body, but in particular, to the core muscles and spine. I recommend approximately 10 minutes as this allows for better mobility in the joints and tissues of the body. It starts to prime the nervous system for activity. It also promotes healing as movement is necessary to bring in the nutrients necessary to heal (if there is already damage or an injury). The cardiovascular warm up will vary and is dependent on your activity or sport.
Dynamic Warm Up
After the initial cardiovascular warm up, progress into a dynamic warm up series. This will typically involve warming up the muscles and joints of the spine, pelvis, and lower legs.
The purpose of the dynamic warm up (specifically in the lower extremity) is to insure adequate mobility in the areas that will be involved in the activity. This will almost always include the hamstrings, hips, and pelvis. Adequate lower leg mobility is important in order to perform your specific exercise or activity. The more motion that can occur through the pelvis and legs, the more force can then be generated and passed through the pelvis.
More mobility in the lower legs and pelvis means less need for mobility in the spine. This means less stress during motion will be placed on the spine—therefore, decreasing your risk of injury. The point is to maximize spinal stability and encourage movement through the hips, pelvis, and upper thoracic.
One example of this is to mobilize your hamstrings by using the foam roller (as demonstrated below).

Spine Specific Warm Up
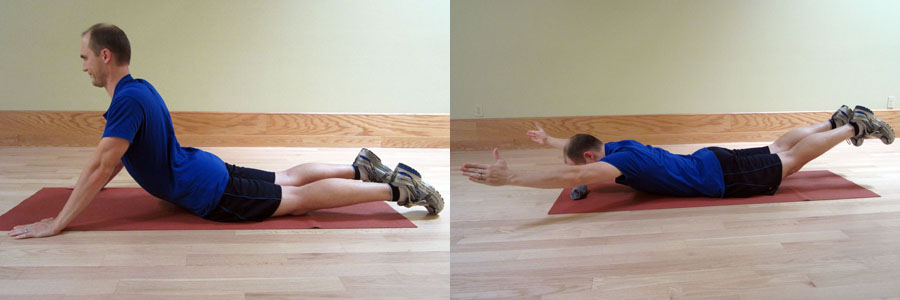
I am a big proponent to performing a very specific spinal muscle warm up upon completion of the cardiovascular and dynamic warm ups. Since you may have already experienced an episode of LBP, a very specific and thorough warm up is important for prevention. Priming the specific muscles of the core (particularly, the multifidus and lumbar extensors) is a critical step to avoiding re-injury. The multifidus is a critical muscle in preventing LBP and must be active to properly stabilize the spine. It helps to prevent shearing forces from affecting the spine which is critical to avoiding LBP.
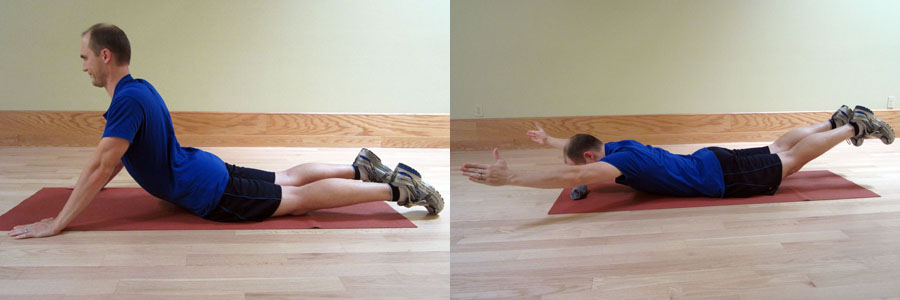
Examples of a spine specific warm up may include performing press-ups and the superman exercise (as demonstrated below).
Sport Specific Warm Up
This warm up will vary significantly depending on the type of endeavor you are about to participate in. For example, a sprinter will need a very different warm up compared to an ultramarathon runner or someone performing in a CrossFit competition. For runners, the warm up varies. Are you racing on a flat course or are you heading out for a very hilly trail run?
It’s important to evaluate the requirements for the event and be ready to perform the actual movements required to compete at a high level. A proper warm up allows your body to immediately perform at its peak and reduces the risk of injury. Regardless of the sport or event, this is also the perfect time to make sure all of your equipment is appropriate for the conditions of the event.
Don’t skip the warm up regardless of your training or event time and/or location! You may be the only one performing a thorough warm up, but it’s because you understand the importance of one in order to prevent LBP and to improve your performance.
It’s important to identify the common mistakes that can cause LBP. By implementing these prevention strategies, you can avoid injury and keep training. Fitness is a lifelong pursuit. If you are injured or just not having fun, then you will not stay engaged and motivated in the long term. Don’t let LBP affect your ability to stay active and keep enjoying your favorite activities!
AVAILABLE NOW ON AMAZON!
In my book, Treating Low Back Pain during Exercise and Athletics, you will learn how to address specific causes of LBP as well as the best practices on how to prevent and self-treat when you experience an episode of LBP. In this step-by-step LBP rehabilitation guide (complete with photos and detailed exercise descriptions), you will discover how to implement prevention and rehabilitation strategies to eliminate pain and get back to training and exercise sooner.
Learn how to prevent, self-treat, and manage LBP so you can get back to your daily life and exercise goals more quickly without additional unnecessary and costly medical bills!
I WANT TO GET RID OF MY BACK PAIN!