In many parts of the world, snow season is upon us. Whether you are shoveling snow or using a mechanical snow blower, your risk of experiencing back pain is likely higher than any other time of the year. If you’re one of the lucky ones who live in a warmer climate, these tips can be just as helpful as you manage those DIY (Do It Yourself) projects.
Whether you’re shoveling snow, working on an outside landscaping project, moving furniture around or just deep cleaning, you’re likely to be exercising different muscles and performing activities that you aren’t used to. Your best laid plans can be derailed by a bad episode of low back pain (LBP). Don’t worry, you can prevent this! If it’s a little too late and you’re already experiencing LBP, I can guide you forward without expensive medical bills, pills, injections or surgeries.
Fortunately, most LBP is mechanical–meaning it’s from a physical or structural cause that is not related to conditions such as cancer or infections. The problem with this type of LBP is that it usually comes back. People who have had an episode of mechanical LBP are 90% more likely to experience it again.
If you’re going to be shoveling that snow or tackling those DIY projects and desire to still be standing upright at the end of the day, it’s best to minimize your risk factors for experiencing LBP by being proactive.

5 Tips to Prevent Low Back Pain When Shoveling Snow:
- Warm up.
Just like any other exercise and/or event, you should warm up first. Pre-activity: A good place to start is to perform standing back extensions and press-ups. This exercise can also very helpful if you are already experiencing low back pain.

- Loosen up.
So many of us sit too much! This causes tightness in the hip flexors and hamstrings. Try stretching your hip flexors and hamstrings.

- Limit the amount of time spent in one position.
This means to limit the amount of time slouched over the shovel or snow blower. Don’t sit or bend over for a prolonged period of time without at least standing up straight (and preferably, performing additional standing back extensions and press-ups as well as stretching your hip flexors and hamstrings). TAKE A STANDING REST BREAK TO STRAIGHTEN BACK UP.
- Use common sense.
If you don’t think you can comfortably lift something, be sure to ask someone for help. If your back is starting to get sore from all that hard work, TAKE A BREAK, but don’t immediately go sit down in a slouched posture. Sitting (especially with poor posture) after working your back really hard is a major risk factor for developing low back pain.
Be sure to work within your limits, and don’t overestimate those limits! Just because you could lift 100 lbs. in high school doesn’t mean that you still can. Always use common sense and proper technique when lifting a heavy object or when performing repetitive lifting and shoveling.
After taking a prolonged rest, be sure to spend a few minutes warming up and loosening up again. Don’t make the mistake of sitting down and resting during your lunch break, only to launch back into the project without making sure that your back is ready. Take the extra time to be certain that your back is ready to start working again.
- Preventing LBP is always best.
Once you have experienced an episode of LBP, you have a 90% chance of it reoccurring. Be proactive! Reoccurrence rates can be impacted and reduced!
Developing adequate strength in the lumbar extensor muscles and core musculature is the primary way to prevent initial episodes and to prevent reoccurring episodes of LBP. Research clearly indicates that the right targeted exercises are the most effective way to manage LBP.
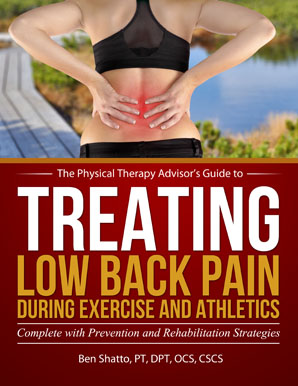
If you’re not sure how to effectively and safely exercise your back or if you’re already experiencing low back pain, I have the solution for you. For the approximate price of just one co-pay to see a doctor, you will receive my easy to read book with step-by-step instructions and a complete video package designed to help you prevent and self-treat reoccurring low back pain episodes.
The Treating Low Back Pain (LBP) during Exercise and Athletics Book and Video Package includes:
Treating Low Back Pain during Exercise and Athletics eBook
In this eBook, you’ll learn why it is critically important to prevent the first episode of low back pain. LBP has reoccurrence rates as high as 90%. If you have already experienced an episode of LBP, you’ll learn why exercise is an important component to long term management. Most importantly, you will understand how to avoid pain and injury in order to take your training to the next level. Topics include:
- Specific strategies for LBP prevention.
- How to address specific causes of LBP.
- Best practices on how to prevent and self-treat when you experience an episode of LBP.
- A step-by-step LBP rehabilitation guide complete with photos and detailed exercise descriptions.
- How to implement prevention and rehabilitation strategies.
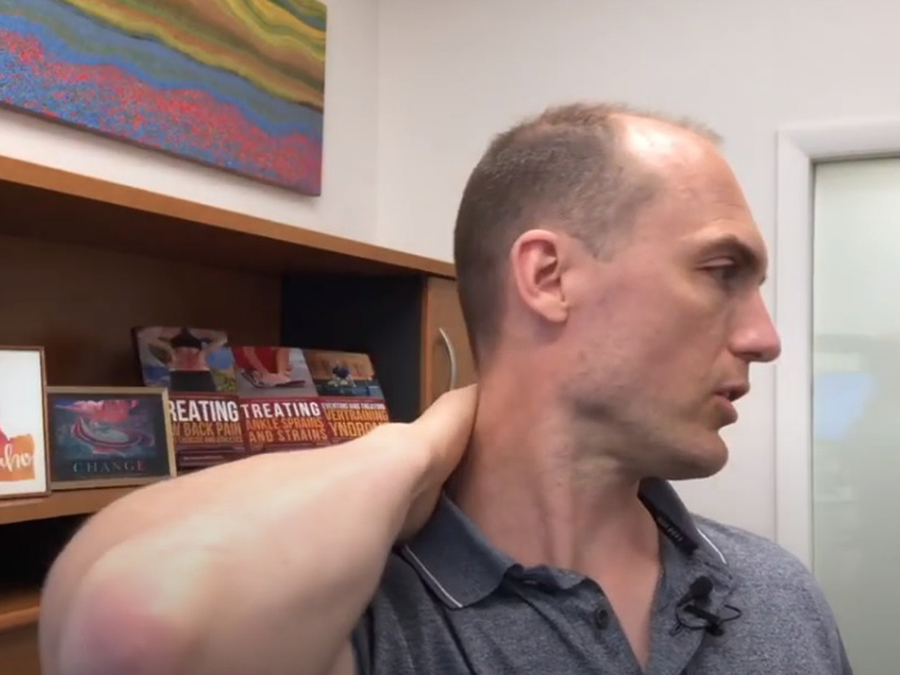
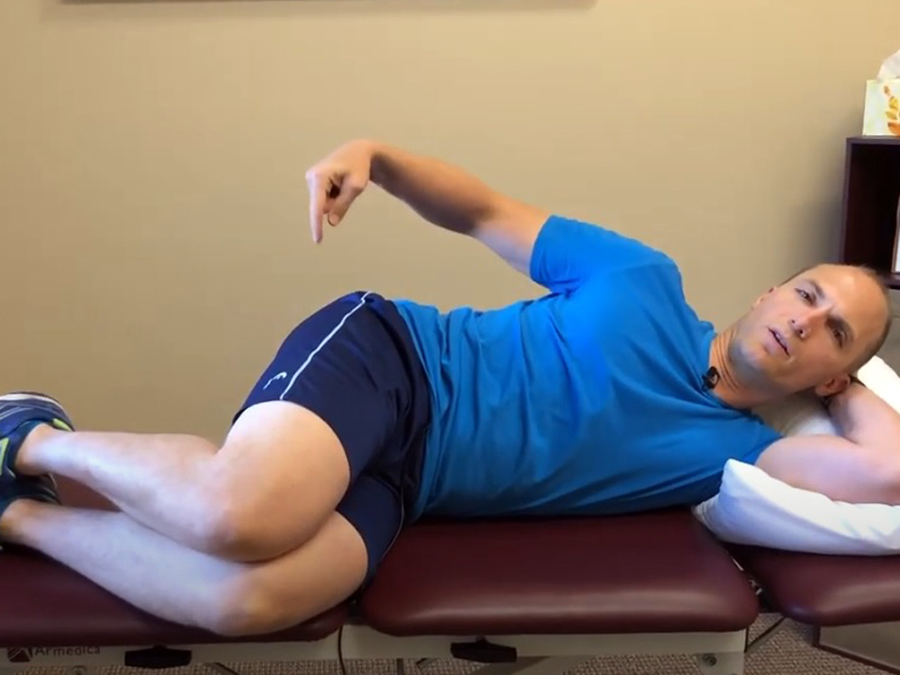
7-part Series of Instructional Videos
Nearly 60 minutes of actionable advice to prevent and treat LBP as it relates to active individuals, sports, and athletics. An in-depth look at treating LBP with a 7-part series of instructional videos in which I address the following:
- Potential Risk Factors for Lower Back Pain
- What are the Core Muscles?
- Prevention during Exercise (Part 1 and 2)
- Initial Treatment
- Further Treatment and Taping
- Long Term Management Strategies and Final Recap
If you have a question that you would like featured in an upcoming video or blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. In case you haven’t already, be sure to subscribe to my e-mail list and YouTube channel as well as join our community on Facebook by liking The Physical Therapy Advisor!