Ankle sprains are a common occurrence and can happen to anyone at any age. The Journal of Sports Medicine (January 2014) conducted a meta-analysis on the topic of ankle sprains. The findings concluded that women were at higher risk of ankle sprains and that children were more likely to sprain an ankle than an adolescent or an adult. Indoor and court sports were the highest risk activity. However, an ankle sprain can occur just as easy from stepping off a curb or accidentally on a pet’s toy. So what is the best course of action to take upon spraining your ankle? Starting with the acute phase, I will walk you through the treatment plan on how to rehabilitate your ankle in this three part series. (If you’re interested in a more complete and comprehensive look at self-rehabilitating an ankle sprain, be sure to check out Treating Ankle Sprains and Strains).
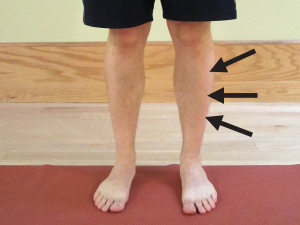
Many different types of ankle sprains are possible, but the most common sprain is known as the lateral ankle sprain. Initially during a lateral ankle sprain, the foot rolls inward (inverts) farther than it should which causes a “sprain” of the lateral ligaments of the ankle. It may also affect the lateral muscles or tendons of the ankle which produce eversion of the foot. The muscles most typically affected are known as the peroneals. In more severe cases, the fibula bone or the fifth metatarsal bone near the pinky toe could also be injured either with a fracture or the tendon could rupture from the bone.
For discussion purposes, I will only address the basic lateral ankle sprain. At the time of injury, a person may often feel or hear a popping sound. This is followed by a fairly rapid onset of swelling in the ankle, typically along the lateral (outside) part of the ankle (near the bump known as the lateral malleolus). This is also usually associated with a significant amount of pain.
Depending on the severity of the pain, the location of the swelling, and any potential bruising, your course of treatment may vary. If you are unsure as to the severity of the sprain, are in severe pain, or you’re not sure how to handle the injury, I recommend that you seek competent advice from a medical doctor, physical therapist, or athletic trainer.
Assuming you don’t have a more serious injury, the initial course of treatment following the sprain includes RICE, which stands for Rest, Ice, Compression, and Elevation.
- Rest – In this case, rest would indicate not using the ankle. I would initially recommend using a crutch or crutches to either fully unweight the ankle (or at least take some pressure off) when walking.
- Ice – Apply ice to the ankle, and the sooner, the better. The rule for icing is to apply ice no more than twenty minutes per hour. Do not place the ice directly against the skin, especially if you are using a gel pack style. Individuals with poor circulation or impaired sensation should take particular care when icing. A bag of frozen peas can be ideal.
- Compression – Compression helps prevent and decrease swelling. Swelling can cause increased pain and slow the healing response, so limit it as much as possible. You can utilize a common ACE wrap or you can purchase a pair of mild over-the-counter compression socks. If you have a friend who is medically trained, many different taping techniques can also assist in decreasing swelling. Many physical therapists or athletic trainers can apply Kinesiology Tape or Mummy Tape for you or you can find application techniques online.
- Elevation – Elevate means to keep the ankle above the level of the heart. This allows for gravity to assist in keeping the inflammation and swelling down. Typically, I would combine the ice with compression and elevation.
Gentle Movement
During the acute phase, move the ankle as much as you can tolerate. I would not be aggressive with the movement. I would not move the ankle if it caused more than a mild to moderate increase in pain. This may irritate the injury and cause more swelling and inflammation. Movement is good and helpful unless it’s causing extreme pain. Focus on the up and down movement of the ankle (known as plantarflexion and dorsiflexion), NOT on the side to side motion (known as inversion and eversion).
Possible Supplementation
During the acute phase, I recommend starting at least a thirty day course of CapraFlex. Capra Flex is an organic glucosamine and chondroitin supplement which also includes an herbal and spice formulation designed to naturally decrease inflammation and support healing. I recommend it to anyone recovering from an injury or attempting to prevent injury when performing at a very high level. I personally use it, and in my practice, it has helped clients recover faster and prevent injury. It can interfere with some blood thinning medication, so if you are on this type of medication, please check with your physician.
The initial acute phase of an ankle sprain can last one to seven days on average. Before progressing into the next phase of rehabilitation, you should be able to stand with equal weight on your feet and not have a significant increase in pain. Once you can, it is time to progress into the intermediate phase (to be covered in Part II).
Knowing how to effectively self-treat and manage ankle sprains and strains is important in order to resume your training and normal activities without the risk of additional damage, injury or re-injury. When you can confidently self-treat, you can limit pain levels, return to activity faster, and prevent reoccurrences.
AVAILABLE NOW ON AMAZON!
In my book, Treating Ankle Sprains and Strains, you will learn how to safely and confidently self-rehabilitate a common ankle sprain. It will guide you through the ins and outs of self-treating your ankle so you can avoid costly rehabilitation bills. Beginning with the acute phase of rehabilitation, I will walk you through the treatment plan on how to rehabilitate your ankle through the intermediate (sub-acute) phase of rehabilitation and return to full activity and sport.
Learn how to safely self-treat and properly rehabilitate your ankle so you can get back to your daily life and exercise goals more quickly without additional costly medical bills!