Q. What are some tips on how to decrease pain caused by spondylolisthesis? -Lisa
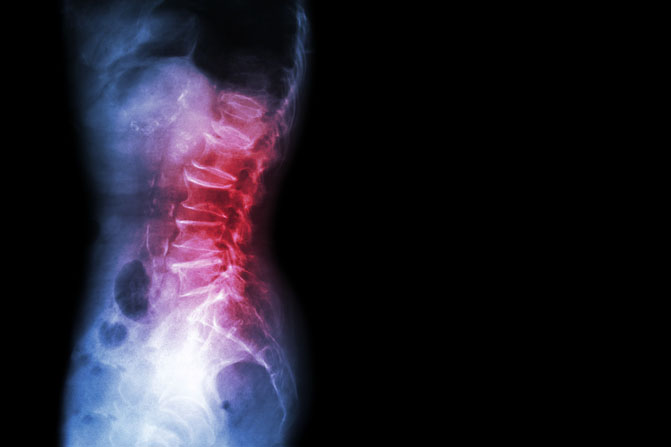
A. Excellent question, Lisa! A spondylolisthesis (spondy) is a certain kind of back injury that is associated with a pars interarticularis defect which is part of the vertebrae. It’s often called the “scotty dog” fracture because of its shape. This condition can be congenital (from birth) or happen from trauma. It’s diagnosed slightly more in males (5% of the male population versus 3% in the female population).
It is important to note if the fracture is stable or not. If the spondylolisthesis is unstable during active motion, such as bending forward or backward, the vertebrae can actually slip and move forward or backward.
Spondylolisthesis injuries are graded I, II, III, IV, and V.
- A Grade I defect occurs when 25% of the vertebral body has slipped forward.
- Grade II occurs when 50% of the vertebral body slips forward.
- Grade III occurs when 75% of the vertebral body slips forward.
- Grade IV occurs when 100% of the vertebral body slips forward.
- Grade V occurs when the vertebral body completely falls off which causes a spondyloptosis.
In many cases, you will never know if you have this particular condition unless an X-ray is taken. For most people, this condition is completely benign and painless (particularly, in Grade I defects).
If you have a Grade I or II spondylolisthesis and are experiencing pain, conservative treatment (including formal physical therapy) is usually the first form of treatment. Surgical intervention may be performed as needed in the case of a Grade II spondylolisthesis. Surgical intervention is almost always necessary in cases of Grade III or higher.
Exercise and Treatment Considerations
In case of a stable Grade I and some Grade II spondylolisthesis, exercise is an important part of the treatment strategy. There are a few items of consideration. First, obtain clearance from your medical physician. Often, a series of X-rays will be taken while you are standing and standing bending either forward or backward. This can determine if the area is stable. If so, then conservative treatment can be initiated.
When determining which motions to guide your treatment, always let pain and directional preference guide your movements. A directional preference is simply a method to identifying a pattern to the pain. Does the pain get worse when you bend over or does it improve? What happens when you repeat this movement? Determine how your pain responds. If it spreads away from the spine and down into the leg, beware that you are moving in the wrong direction. Stop that particular movement. If the pain improves then continue with exercises in that direction. Never do anything that worsens your pain or symptoms.
On average, I tend to have my clients be less aggressive with lumbar range of motion, especially press-ups and backward bending. Although it’s not prohibited completely in the case of a stable injury, it’s merely a precaution as some research indicates that it may have the potential to cause more pain and worsen the pars defect.
It’s also entirely possible that the cause of pain has nothing to do with the spondylolisthesis. A thorough physical therapy evaluation should help to determine the actual cause of the pain (although, sometimes it is never truly known). The American Physical Therapy Association (APTA) offers a wonderful resource to help find a physical therapist in your area. In most states, you can seek physical therapy advice without a medical doctor’s referral (although it may be a good idea to hear your physician’s opinion as well).
The focus of the treatment and exercise is on the strengthening of the inner and outer core muscles and lumbar extensors. With the only caveat being that you may need to avoid excessive loading with the spine extended. In this instance, I recommend that you work with a highly qualified trainer or sports medicine professional to insure that you are performing your particular exercise and sport in a manner that will keep you safe and the fracture stable.
It is also important to insure proper hip and pelvic mobility so that the spine is not over worked. In cases of spondylolisthesis, insuring a normal amount of hip extension in addition to proper hamstring length and hip rotation is important. If the hip cannot fully extend during walking and running, it will cause excessive lumbar extension. You may even want to focus on having less of a lumbar curve (a posterior pelvic tilt) if your tendency is to hyper extend with an anterior pelvic tilt. Be sure to work on thoracic mobility to insure the entire vertebral chain can move freely.
Exercise is the critical component to the management of this condition. I would highly advise that you consult with a local physical therapist that has a Lumbar MedX exercise machine. This particular machine can isolate the lumbar multifidus during exercise better than any other exercise that I am aware of.
Other exercises can be utilized to activate the multifidus. These Lumbar Extensor Exercises are designed to progressively activate the multifidus muscles (with the final exercise being the most challenging). Generally improving your core strength is a critical component to the overall treatment. My only caution is to once again avoid excessive loading in hyper extension and to take your strength progression more slowly while monitoring your symptoms. If you perform an activity that causes worsening pain, then you will need to modify or eliminate that particular activity until it can be performed pain free.
In some cases, more flexion biased stretches would be indicated. This would be determined by the directional preference. If extension biased exercises worsened the pain and flexion biased exercises improved the pain, then initially you would proceed with flexion biased exercises to help control pain while you progress into your core and lumbar stabilization program. Examples of flexion biased stretches would be a single knee to chest (below left) or a double knee to chest exercise (below right). Hold these for 20-30 seconds at a time and perform 4-5 repetitions each.
Good luck, Lisa! I hope you find this information to be helpful and provide some relief from the pain you’re experiencing. For more information on treatment strategies for low back pain, please refer to How to Safely Self-Treat Low Back Pain.
Do you suffer from spondylolisthesis? Please share your best tips for pain management.
If you have a question that you would like featured in an upcoming blog post, please email contact@thephysicaltherapyadvisor.com. For additional health and lifestyle information, join our growing community on Facebook by liking The Physical Therapy Advisor!
Disclaimer: The Physical Therapy Advisor blog is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice. No health care provider/patient relationship is formed. The use of information on this blog or materials linked from this blog is at your own risk. The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Do not disregard, or delay in obtaining, medical advice for any medical condition you may have. Please seek the assistance of your health care professionals for any such conditions.