I must warn you that this is not the typical post from me. All of the information is true and sadly, not exaggerated in any way. My hope in documenting this true account of events is that it will help others know how to better avoid injury. If you do develop an injury, then maybe some of my self-treatment strategies could be helpful.
What most people don’t know about me is that I have struggled with low back pain (LBP) for over 20 years. Early on, I had years of constant and chronic LBP. This pain helped drive me to seek out different self-treatment methods. I began to understand LBP along with the best practices on how to self-manage and most importantly, avoid future flare-ups. This has personally helped me manage my own pain while helping thousands of others either directly with physical therapy or by sharing my book, Treating Low Back Pain during Exercise and Athletics.
Even with all my diligent efforts (most of the time), the occasional LBP flare-up occurs. Unfortunately, the last incident was due to poor judgement on my part. In early November of last year, I had been sitting a lot while working on a few projects, and my back started to ache. It was mild at first. However, by mid-month, I could hardly get out of a chair and walk.
As a physical therapist (PT) that specializes in treating LBP, I should have known better, but I chose to do what most people do. I ignored it, and pressed on. I reminded myself that I’ve had this pain before, and it typically goes away. Right then, I didn’t have time to address it.

Monday morning rolled around, and I was scheduled for my 5 mile tempo run. As any runner or exercise enthusiast knows, if it’s scheduled, then it must be done (no matter what, right?). I was sure my back would loosen up as I ran. Often times, a warm up prior to running makes it feel better. (If I was being honest, the pain was pretty bad that particular morning. It was preventing me from sitting, getting out of my car, and even walking straight. Was that a good enough reason to cancel a run?)
I managed a short walking warm up since that was all I could muster and proceeded into a slow jog. About 2 miles into my jog, my right calf started to hurt. Why stop? I was sure it would all shake loose soon…
As mile 3 approached, I was falling apart. My back hurt to the point I couldn’t stand up straight. My right calf was completely locked up. It was giving me a sharp pain with every step. The bottom of my left foot started aching. I finally shut it down and limped home.
Later that day, my calf wasn’t any better (neither was my back), and now I had full on plantar fasciitis. Pretty good start to the week, but I got that run in. By the end of the day Monday (post run), I was miserable, but I didn’t dare tell anyone.
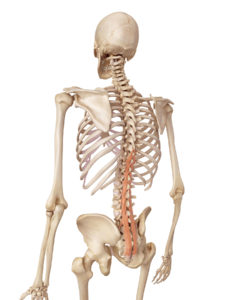
As a PT, I should have known better. I started to analyze exactly what was going on. For some reason, my disc bulges (a pre-existing problem at L4/L5 and L5/S1) had flared up for no apparent reason and were hurting terribly. My back pain had caused a left lateral shift in my spine, which meant I couldn’t stand normally. The nerve tightness down my left leg affected my walk, so I could not fully stride out.
In hindsight, my sad attempt at a run early that morning was actually a terrible idea! I had obviously been running with a poor gait pattern. This altered gait pattern with poor running mechanics resulted in a right calf strain and the development of plantar fasciitis in my left foot. (And this all started in 3 miles!)
My initial treatment was to determine my directional preference for my lumbar spine pain:
A directional preference is a way to identify a pattern to the pain. Does the pain get worse when you bend over or does it improve? What happens when you repeat this movement? Determine how your pain responds. If it spreads away from the spine and down into the leg, beware that you are moving in the wrong direction. Stop that particular movement, and instead try moving in the opposite direction. If you were moving into flexion, try extension. If you had trialed extension biased movements, try flexion. Find the movement pattern that helps the pain improve and that has a positive effect on any other symptoms you may be having.
I determined my directional preference. As I performed my series of movements, my symptoms were peripheralizing (returning back to the middle of my back to the point I could stand straight and walk normal).
After a series of 10 side glides followed by 10 press-ups (as demonstrated below), I could eliminate 75% of my LBP and symptoms as long as I didn’t sit. Sitting would immediately bring the pain back on. For the next several weeks, I avoided sitting at all costs including during dinner.

I also started back extensions over an exercise ball (3 sets of 15 repetitions as demonstrated below) every morning as part of a lumbar strengthening program. I chose back extensions to insure that I was working my lumbar extensor muscles. I kept my movement patterns within my directional preference. This was preceded by and followed by side glides and press-ups as well as continuing to avoiding sitting. I stopped running since I couldn’t fully walk or jog without an altered gait pattern.

For my calf, I started foam rolling and stretching regularly. I used a mobility band (as demonstrated below) as a way to provide compression while I performed heel raises (typically a set of 20-30 repetitions). Thankfully, I had the opportunity to trial a product that not only utilized the compression from the mobility band, but added a way to self-mobilize the calf. The CTM Band worked exceedingly well for this. (“CTM” stands for compression, tension, and movement.) Use code MTA15 for a 15% discount. (If you suffer from any form of blood clotting disorder or are on blood thinning medications, I would advise against utilizing mobility bands for any type of deep compression.)

For my plantar fasciitis, I also performed calf stretches as well as used a small ball (as demonstrated below on the left) to mobilize the bottom of my foot. Pain in the morning seemed to be the biggest issue, so I would sit up and stretch before getting out of bed (as demonstrated below on the right). By the end of the day, my foot would really start to hurt. Since I was unable to sit due to my back, I used a padded stool to kneel on whenever possible.

I continued this treatment plan for over 3 weeks. For the first 2 weeks, I was unable to run, so I concentrated on rehabilitation exercises only. During this time, I utilized a self-prescribed course of over-the-counter Ibuprofen (anti-inflammatory). I didn’t have any medical issues with taking this medication. Please consult your physician before taking any medications or supplements.
I also initiated a supplementation protocol consisting of adding collagen hydrolysate to my daily smoothie as well as taking CapraFlex by Mt. Capra. (It combines an organic glucosamine and chondroitin supplement with other natural herbs and enzymes which are designed to reduce inflammation, promote bone and joint healing, and wellness.)
This continued for approximately 4 weeks. The rationale behind the supplementation was to insure that my body had the necessary building blocks to heal and to provide additional anti-inflammatory support to my body during my recovery.
After 3 weeks, I returned to running for only shorter distances (under 5 miles). I was tapering back into other exercise routines with appropriate modifications which included increasing my warm up and cool down times and avoiding bending forward since I wasn’t 100% better.
The reason I chose to share my most recent LBP episode with you is because I have heard versions of this story over and over again from other runners, weekend warriors, and patients. We really can be our own worst enemy!
As a PT, I should have known better than to run that day. As a runner and weekend warrior, the feeling that it may be a “mortal” sin to miss a scheduled run or work out can be a powerful temptation to do it even though your body may be telling you to reconsider.
As any frequent exerciser knows, a few aches and pains is par for the course. In fact, it’s pretty normal! Oddly, I will have just as many if not more, aches and pains when I stop running and exercising as when I’m regularly training.
The moral of my story is a reminder to be very self-discerning and self-aware to understand what is a typical ache and pain versus something more serious. In my case, not being able to walk normally due to pain should have been a clue not to run abnormally either. My abnormal running pattern that day is what led to the overuse injuries in both my calf and foot. What was surprising even to me was how fast the pain developed and turned into a true overuse injury in only the course of 3 miles!
If you’re not sure how to effectively and safely exercise your back or if you’re already experiencing low back pain, be sure to check out my Treating Low Back Pain (LBP) during Exercise and Athletics Book and Video Package.
Treating low back pain does not need to be difficult or expensive. For the approximate price of just one co-pay to see a doctor, you will receive my easy to read book with step-by-step instructions and a complete video package designed to help you prevent and self-treat reoccurring low back pain episodes.
USE DISCOUNT CODE LBP AT CHECKOUT FOR 15% OFF!
SAVE 15% NOW!
If you have a question that you would like featured in an upcoming video or blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. In case you haven’t already, be sure to subscribe to my e-mail list and YouTube channel as well as join our community on Facebook by liking The Physical Therapy Advisor!