Preface: This blog post is much different than anything we have shared before. It’s a deeply personal experience from my dear wife, Alana. It touches on her near death experience and her interaction with our local health delivery system. It also exposes the problems with the response that has been taken to deal with COVID-19 pandemic. I feel that some of the response our healthcare system has decided on is definitely not in the best interest of the patient.
I often write about resilience and how it’s not just a physical characteristic. It’s comprised of emotional (psychological), mental (cognitive), social (relationships), and spiritual characteristics that are all important to one’s health and recovery. Our healthcare system is great at saving lives, but may have forgotten that these other characteristics of resiliency are just as important as the physical component to recovery.
In her recount, Alana gives strong praise to the surgeon and the team. The nursing staff did their best, but was overburdened. (It placed extra stress on them since a family member couldn’t be in the hospital room to support the patient during the COVID-19 restrictions.)
My plea for any healthcare worker out there that may read this: don’t forget the patient! You’re in healthcare to help people. We cannot neglect the mental state of our patients if we hope to have positive long term results. Let’s find a better way to keep everyone safe and to really help those in need. Our patients are likely in their darkest hour.
Humans, people, and your loved ones are complicated and so is their health. It’s not just the physical aspect of things. It’s also the emotional, mental, social, and spiritual aspects that make up a person that dictate how he/she will physically heal. It’s not just what we do for a person; it’s how we make them feel that will stick with them for a life time. There is never too much compassion for those in need. Thank you for your continued service in tireless work that you’re often not acknowledged and thanked for!
By Alana Shatto
Thurs., 5/14/20
On Thursday morning, I enjoyed a mushroom coffee blend for the first time at breakfast. Not thinking too much about it, I started getting a stomachache by lunch time to the point that I couldn’t eat. After sitting, I had trouble walking around the house. I lied down in my bed with a racing heart and chills (which was unusual for me since I can typically just push through). Ben brought home dinner, and I was able to eat. Although tired, I went to be at 9 p.m. thinking I would be just fine.
Fri., 5/15/20
I tossed and turned most of night. My heart felt like it was racing, and I had the same right calf pain that had been bothering me most nights (I struggle with tight calves and achiness in them at night). Ben got up at 5:15 a.m. to get ready for CrossFit. At about 5:35 a.m., I called out for him several times. I had severe shaking and chills, and I was having trouble breathing. Long gasps for breathe. He took my temperature, 99.1 degrees. He then got out his pulse oximeter, and my heart rate read at 150-160 beats per minute. Very alarmed, he told me that we needed to go to the emergency room (ER) and that he’d go wake up our ten year old daughter, Alexis, to get ready to leave.
He had to help me get dressed to leave. I could hardly think clearly. I could barely walk and make it out to the car. I tried to drink bottled water, but threw it up into a bag as we drove to St. Luke’s Meridian ER in the cold darkness of the morning.
Because of the COVID-19 pandemic, we had to wear masks. Ben told me that I would have to do this alone. He told me that they would be running an EKG and all of these tests to figure out what was wrong. He was sorry that he couldn’t be with me because of the visitor restrictions due to COVID-19.
I don’t really remember saying goodbye to Ben and Alexis nor did I grab my phone thinking maybe he put in my fleece jacket pocket. They wheeled me away in the wheelchair, and things got really crazy (fast)!
The fully masked staff asked me a lot of questions as they began to put in an IV in my wrist and my left inner elbow. They started hooking my body up for an EKG to check my heart. I told them about the mushroom coffee that I had drunk the day before and the symptoms from the day before. It was difficult to breathe in addition to wearing a mask and fogging up my glasses as I tried to calm down.
I was sure I had COVID-19 and would be one of the random younger adults that suffered from cardiac arrest due to it. I thought to myself, “This is the end. I’m going to die alone.”
I could hear the whispers in the hall of the staff going over my symptoms. A man’s voice asked, “Did you hear her cough?”
I thought back earlier in the year…
Alexis, always healthy and strong, had gotten sick on Valentine’s Day, 2/14/20. Over the following six weeks she was diagnosed with adenovirus, pink eye, mono, and an ear infection! A crazy series of illness that kept us home long before the quarantine / stay at home order. I had wondered if we had already had COVID-19, just before all of the fear and testing. I thought this was it; we were through all the illnesses. I had thought we were on the up and up…just in time for summer.
Over the course of the next few hours I was tested for the following:
- COVID-19 – Rapid 30 minute testing in which a nurse shoved a 14 inch long looking swab up into my left nostril until it hit the sinus cavity.
- Cat Scan – Chest view as they suspected a blood clot in my lungs or possible pneumonia.
- Virus Swab – Another test in which a nurse shoved a 14 inch long looking swab up into my right nostril until it hit the sinus cavity. She later came back to tell me that there was a problem with the swab, so I bared it again in my right nostril for a total of three times.
- Cat Scan – Abdominal view as they hadn’t quite figured out the source of the infection.
- EKG – Second test to confirm that my heart was functioning and not enlarged.
Of course, all of these tests take time as I’m wheeled on the hospital bed back and forth to get the CAT scans. It’s one heart pounding moment after the next…
“You might have a blood clot in your lungs or you may have pneumonia.”…BUT YOU DON’T.
“You might have COVID-19.”…BUT YOU DON’T.
“Your heart is fine—normal and not enlarged.”
Probably between 9 and 10 a.m., the radiology report came back that they had found the source of the infection:
APPENDICITIS
“Whoa, what?!” Where did that come from?
The ER doctor continues on to say that I have an inflamed appendix and that it needs to come out. There is no other treatment—just surgery.
I think we were all a bit dumbfounded as I didn’t arrive in the ER with right lower quadrant pain, so I wasn’t fitting the medical diagnosis for appendicitis.
After all of the ups and downs, I wasn’t sure about how I felt about going into surgery alone. I knew I didn’t have a choice. I had only been under anesthesia once before for my wisdom teeth to be pulled. I had only been to the hospital to deliver Alexis (natural childbirth). Why at 41 years old am I sitting in the ER with appendicitis?!
“This is the end,” I thought to myself. I’m going to die alone and not even have a phone to call on.
Luckily, at that point the nurse gave me the hospital room phone to call Ben once we discovered that I didn’t have my iPhone in my fleece jacket pocket after all.
The ER doctor had called Ben previously, so he somewhat knew what was going on. I was able to tell him myself about the appendicitis and the surgery. We spoke a few times before I was moved to Pre-Op. At that point, we knew that they were admitting me into the hospital.
Although the staff at Pre-Op was caring, things got worse after giving a urine sample (to make sure that I wasn’t pregnant). I started getting chills no matter how many warm blankets I was given. Between talking to the anesthetist and the surgeon, I was nauseous and dry heaving.
Finally by 12:30 p.m., I was wheeled into the operating room and transferred to the table.
I don’t remember anything after that besides music playing the background.
When I came to, I was struggling to breathe. The breathing tube was still in my throat—I couldn’t move my left hand or speak…An orange plastic cover was over my face. Then things went black again.
I woke up in the recovery room after that. It was likely after 3 p.m. At some point, the surgeon came in to speak with me. He told me that they had removed my appendix, but that there was vein that ran along side of the appendix that had pus which had been sending bacteria through my bloodstream and the appendix was leaking into my abdominal cavity, sepsis! They had cleaned out my innards with saline and an antibiotic solution and had given me 6 liters of fluid since coming to the ER to keep me alive. I would stay at the hospital with intravenous antibiotics.
I don’t remember too much about Fri. night other than I cried on and off. Overnight, I experienced chills, shakiness, and changes in my breathing. Although the night shift nurse consoled me by telling me that this was common with sepsis and after surgery, I felt utterly alone. Again, with the COVID-19 pandemic the hospitals are not allowing any visitors at all.
God was silent though I continued to pray. The darkness of the night overwhelmed me. I was experiencing nighttime terrors. I saw black flashes and movements throughout my empty hospital room. When I closed my eyes, I saw the cloaked Grim Reaper face. I jolted in and out of rest. Darkness like a black ink spilled surrounded me…
Sat., 5/16/20
The morning went poorly. I cried with the surgeon when he came by making his rounds. He had warmth about him and a caring spirit. He told me to expect a three to five day hospital stay.
My best friend Mandy called me on the hospital room line before noon, and I wept with her. I also spoke to my mother-in-law, Debbie, who encouraged me and prayed over me. I spoke briefly to my parents, but the hospital telephone line was low and muffled, making it difficult for people to hear me and for me to hear them.
Once Ben knew that I was staying, he arranged a drop off of my phone and a change of clothes to wear home at some point. He had to package everything up in a plastic bag and drop it off with the guard station at the hospital. Although he was physically there, he could not come to room to see me, encourage me, and pray with me because of the visitor restrictions due to COVID-19. My mental health upon arrival up until now remained poor as I felt so alone.
It was an instant boost in moral to have my phone again and to be able to text. Now I didn’t feel as alone.
In the afternoon, I walked the hospital hallway slowing pushing my IV machine. I started to feel better, but how strange it was to walk the halls of the 6th floor wing and see all these other patients alone in their rooms and in their beds…no friends, no family, no support.
I had previously heard Code Gray announced over the hospital’s public address system, possibly indicating the need for an emergency management response to a combative person with no obvious weapon. I had also heard Code Blue indicating a medical emergency, possibly involving cardiac or respiratory arrest. My heart broke for these patients as they were miserably alone as well.
I dreaded the darkness of the approaching evening…
Early morning on Sun., 5/17/20
Although exhausted and not feeling well, I drifted off to sleep in-between the nurses waking me up to check my vitals or to replace my IV bags with medication. The night terrors returned after 2 a.m.
I laid silently in the hospital bed with tears streaming down my cheeks. I sang, “Come, Holy Spirit.”
The lines of the song, “Way Maker”, filled my head:
You are
Way maker, miracle worker, promise keeper
Light in the darkness
My God, that is who You are
I called out upon the name of JESUS to reprimand the evil spirits. Quiet tears streamed down my face.
Jesus’ voice told me to call out for prayer…breaking the silence I had endured.
I put on my glasses and grabbed my phone. I fumbled to Vineyard Boise’s Facebook page and started my prayer request:
“Prayer request: I had emergency surgery to remove my appendix on Friday. I was already sick beforehand, but I had no idea that I had a serious infection. I have sepsis, bacteria in my bloodstream. Because of COVID-19, no hospital visitors, so Ben and Alexis can’t be here with me. Please pray for healing and a complete recovery so that I am strong and can go home to be with my family. Thanks”
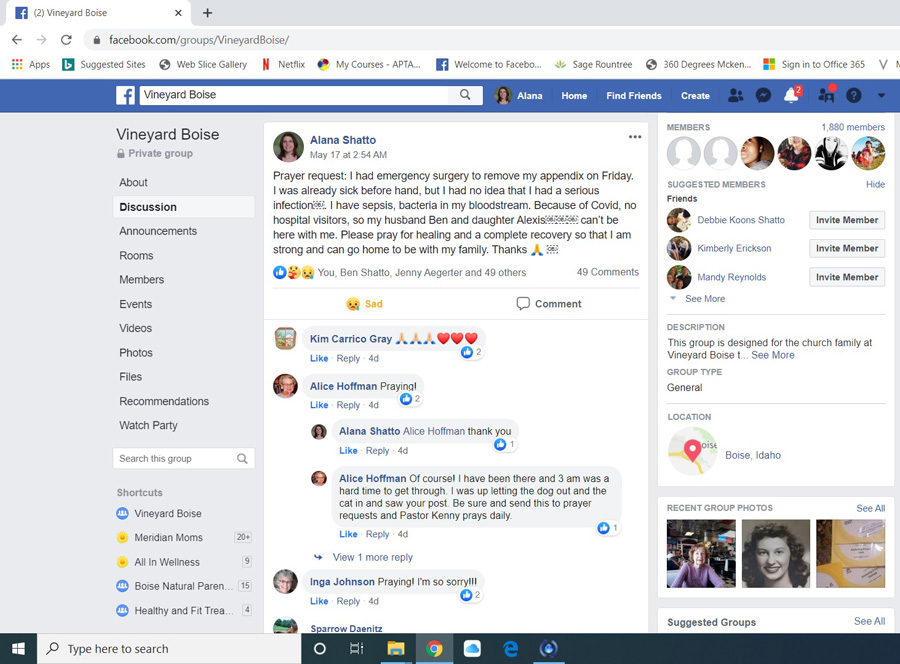
Within in moments of publishing, I was surprised to see that a couple of ladies had already responded and starting praying for me! Wow—people really are awake and on Facebook at all times of the day! Hopeful, I shared the same call for prayer on my personal page.
Setting my phone aside, I laid there thinking, “OK, at least two people are praying for me, and I’m not alone.”
I felt a presence of an invisible scan come over me. It started above my head and traveled across my body to my toes. It was like a sheet pulled off of me from top to bottom. He knit me back together. And I felt peace and drifted off to sleep.
6 a.m.
The hospital room lights glared on! The blood lab technician stormed in (like the previous morning without warning or easiness) with his equipment to draw my blood. I was startled awake.
After he left, I popped up out of the hospital bed and start my bathroom routine. I ordered my breakfast (vanilla pudding and hot tea) at 7 a.m. and was sitting down to eat when the nurse came in.
She was surprised to me eating at the shift change. She said she’d never seen anyone up like that before.
I was up and around until about 10 a.m. I walked the hallway pushing my IV machine. I felt like I had turned the corner. I felt like myself again.
By 11 a.m., the surgeon and his physician assistant (PA) came by during their rounds. The surgeon reported that my 6 a.m. blood test results had come back completely normal! The white blood count was normal. I was only minor low on potassium.
He had expected me to stay in the hospital at least through Mon. and possibly until Wed.
He told me that he had been practicing since 2006 (14 years) and never seen a case like mine before. I was in serious sepsis shock prior to surgery to remove my appendix. They had to pump me full of 6 liters of fluid to keep me alive.
If I hadn’t have come to the ER when I did, I would have died. Ben could have left for CrossFit. I could have died alone in bed while Alexis was asleep in her room.
The surgeon and his PA were warm, caring, and encouraging. He discharged me from the hospital on Sun. afternoon. We addressed my swelling: my stomach, thighs, and ankles were very puffy. He told me that I’d pee out all of the fluid within a couple of days.
I was able to independently shower, dress (though my normal clothes felt tight), and pack my own belongings. I made sure to request my medical records for the hospital stay.
Ben and Alexis got all of my prescription medication (including an 8 day course of two antibiotics) and met me at the hospital parking lot sometime after 3 p.m. It wasn’t all smooth sailing after that. I had nausea from being pushed (way too quickly) in the wheelchair, being in the elevator, and during the car ride home to the point that I had to take the anti-nausea medicine in the driveway.
It wasn’t until I saw my picture that Ben took of me at the hospital, that I realized how swollen, fat, and ugly I felt, but I was alive. It hadn’t dawned on me that I was having trouble moving around due to the water weight gain. Turns out I put on 15 lbs. of swelling while hospitalized. I was worried about how Alexis would “see” me after such a traumatic event for her to witness.
It was later that day that I found out that Ben awoke at that same time (Sunday morning at 3 a.m.) to what sounded like dropping marbles, so he laid awake in bed praying for me. My brother-in-law and sister in-law were awake with their almost 2 ½ year old praying for me at the same time. It turns out that hundreds of people (I didn’t even personally know) began to pray on my behalf throughout Sun.
I won’t lie and say that everything was fine after that because it wasn’t. I had jittery chills and a terrible night of sleep. I was worried about my breathing and my heart rate and that I’d have to go back to the ER. I second thought my decision to come home—knowing the stress and pressure it placed on Ben and Alexis.
Mon., 5/18/20
That Mon. morning, God met me in my devotions that I get automatically emailed every day. It was exactly what I needed to hear, and it encouraged me to keep going.
But he knows the way that I take; when he has tried me, I shall come out as gold. My foot has held fast to his steps; I have kept his way and have not turned aside. (Job 23:10-11)
Later in the day when Ben heard me sneeze or cough, he couldn’t believe that I didn’t have pain my abdominal area. He said that he figured I would be doubled over in pain, but I wasn’t. I told him that I couldn’t believe it either. I truly believed that God had knit me back together.
Thurs., 5/21/20
Unfortunately, I hadn’t lost any of the swelling within the predicted time frame. After speaking with the surgeon’s nurse, I was given a three day course of Lasix, a prescription diuretic that causes you to pee more in order to help your body get rid of extra water.
During that phone conversation, I was given the pathology results: no cancer and no tumor were found in my appendix. The bacteria culture showed that I had an E. Coli (a type of bacteria that normally lives in your intestines) infection. I was on the correct antibiotics to treat the infection.
Luckily, the Lasix worked and by Sun., I had lost 19 lbs. and had minimally swelling in my feet!

LEFT: Sun., 5/17/20 Hospital Discharge with 15 lbs. of water weight gain. RIGHT: Sun., 5/24/20 One week later and 19 lbs. lighter!
In summary, my recovery has been slow and steady. The three laparoscopic incisions on my lower abdomen are slowly healing. The bruises are fading. The nurse said that it could be another one to two weeks before I have my energy and appetite back. I know I’m on the right track though the CAT scan showed that I have a nodule on my thyroid that needs to be further looked at by ultrasound. My thyroid lab tests result fell within the normal range, but it needs to be further followed up with my general practitioner.
It was the worst time amid the COVID-19 pandemic to have an emergency surgery and lonely hospital stay without Ben or Alexis, but I made it and truly appreciate all of the prayers and support we have received…Family and friends brought delicious meals, beautiful flowers, and get well cards. I appreciated the encouragement amidst the struggle.
My story did not end on 5/15. I was lucky to have been given another chance as I know that many others in the hospitals, nursing home, and assisted livings have faced death alone with family outside the window or building because of COVID-19 restrictions. I’m truly sorry for those who have endured such horrendous circumstances.
Although I am still grappling and processing through all that has happened, I have gained a fresh clarity of what is important and what I need to let go of. I hold my relationships with family and friends dearly to my heart. I let go and released my hand of anger, control, and perfectionism. It no longer served me. I feel as though I have been given the opportunity to push a giant “RE-SET” button. I’m more mindful of my thoughts, behaviors, and even the food I’m willing to reintroduce. I have given up my coffee for now as the caffeine seems to directly affect my heart rate at rest, causing it to push near 100 beats per minute, where 60 is typically normal for someone my age.
Should you find yourself or a loved one in a similar situation one day, I hope my honest and candid sharing of my health journey might help you or your loved one through the process. Mental and spiritual health is so important to recovery and resilience. Forced solitude is very difficult to bear even in short situations and especially, when battling an illness. Any kind of interaction is precious and helpful.
Hold fast. Stay strong.
Take the time to focus on your health and recovery. Often, small changes in your diet, activity level, and relationships can make a big difference. You can take control of your health and your life!
Reach out to others for support. No matter how you feel or where you find yourself, YOU ARE NOT ALONE. God Bless You!
Remember what you’ve learned about the Lord through your experience with Him. (Deuteronomy 11:2)
If you do that, our messes will become our messages.







 About Dr. Matthew Crooks
About Dr. Matthew Crooks