Do you have pain between your toes? Does it feel like you are always standing on a pebble or have a lump in your socks between your toes? This may be Morton’s neuroma. A neuroma is a thickening of the tissue that surrounds the digital nerve bundle. Morton’s neuroma is one of the most common types of neuromas and typically occurs between the third and fourth toes.
Morton’s neuromas occur due to repeated stresses, irritation, and/or pressure at the ball of the foot which affects one of the nerves that leads to the toes. There typically isn’t any swelling, bumps or bruises with Morton’s neuroma. Learn how to determine if you have Morton’s neuroma in your foot and how to self-treat it.
Morton’s Neuroma Symptoms include:
- Numbness or tingling which is affecting the ball of the foot, between the toes, and/or the toes themselves.
- Sharp, stabbing and/or burning pains that are intermittent and only affect either the ball of the foot and/or toes (usually the third and fourth toes).
- The sensation of standing on a pebble or marble or having a lump in your shoe or sock.
- When running, the pain is often felt during the push off from the toes prior to the swing through phase.
Common Risk Factors for developing Morton’s Neuroma:
- Sports and activities that involve repeated impact affecting the feet (such as jogging and running sports).
- Poorly fitting footwear. This is particularly true for high heel shoes, but it’s also very common in athletic and running shoes. Most commonly, the toe box is too small. A sole that is overly flexible in the wrong location can cause excessive give in a location which isn’t in proper alignment with the metatarsals of the foot.
- People with common foot deformities, such as bunions, hammertoes, flat feet or overly high arches, are at risk for developing Morton’s neuroma.
- Poor ankle mobility, particularly excessive tightness in the Achilles tendon or calf muscles.
- Poor foot muscle strength, particularly the foot intrinsic muscles which help to support the arch of the foot.
- Women are eight to ten times more likely to develop Morton’s neuroma. High heels are a likely culprit.

Do I have Morton’s Neuroma in my Foot?
Morton’s neuroma is often diagnosed through a physical examination and imaging. However, a very thorough history and physical examination can be quite conclusive. The imaging is typically only to rule out other possible causes of the pain such a stress fracture.
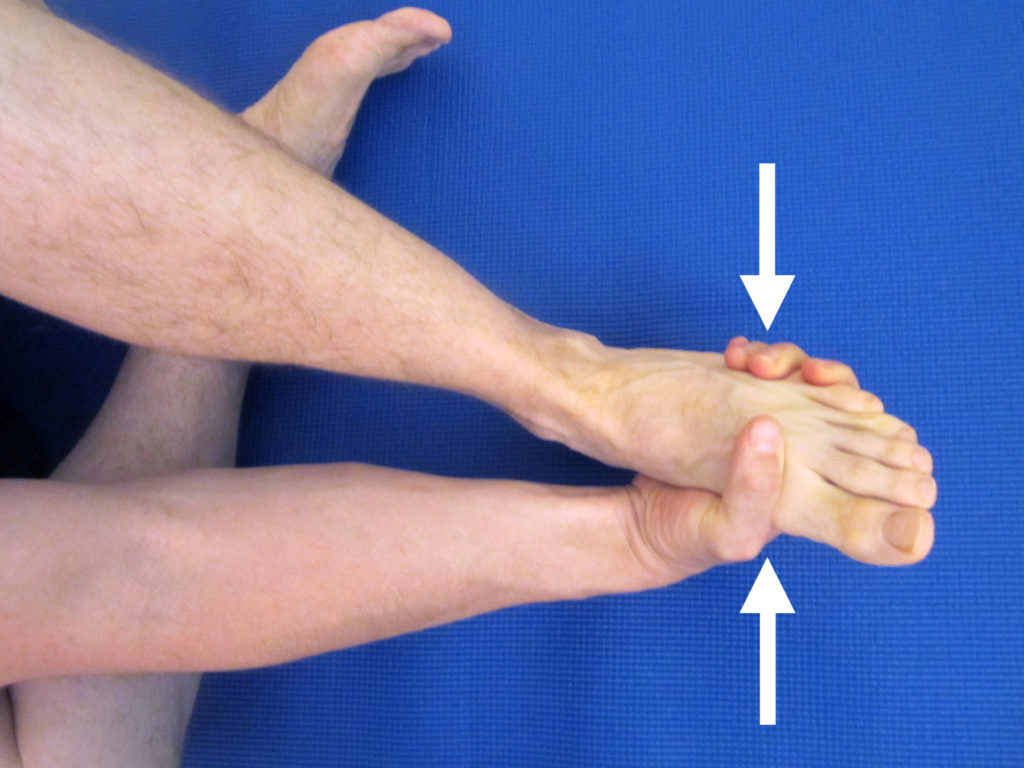
The physical examination includes palpating between the toes. The painful area will feel “thicker” on the affected foot in comparison to the other. There is often an associated clicking of the bones when the area is squeezed or moved back and forth. When the forefoot is squeezed and held for several seconds for a Morton’s Neuroma test, it will often reproduce or worsen the symptoms of burning and or tingling.
How to Self-Treat Morton’s Neuroma:
Avoid wearing tight fitting, ill-fitting, and high heeled shoes. Be sure that your shoes have an appropriately sized toe box. In the case of athletic shoes (particularly, for distance running), extra room in the toe box can be beneficial as the foot will often swell during the course of the run. If you wear high heeled shoes, consider wearing them less frequently and/or switching to a shorter heel. Even wearing socks that are too small can potentially cause too much compression and lead to increased symptoms.
Orthotics. Many people respond well to a rigid orthotic with an extension underneath the first metatarsal bone. You may not necessary need custom orthotics. Many running stores sell an over-the-counter orthotic such as Superfeet Blue Premium Insoles. The blue tends to fit most feet, but a variety of options are available for customization. In my experience, these insoles can last 1,000 to 1,500 miles easily. If the over-the-counter options aren’t helping you, please see a physical therapist or podiatrist for custom orthotics. Seek assistance from a professional who is a runner and has experience with treating other runners.
Metatarsal buttons and pads. Adding a metatarsal button or pad may be enough to spread out the metatarsal heads and alleviate the pain for those who don’t want a full orthotic. Although often a metatarsal pad may be incorporated into a custom orthotic. I recommend these Pro-Tec Athletics Metatarsal Pads.
Anti-inflammatories. Initially an anti-inflammatory may be necessary. Speak to your physician about the best type of anti-inflammatory for you. In severe cases, a cortisone injection may also be warranted. However, you must address the biomechanical causes for the pain in order to prevent it from recurring.
I am a supporter of natural supplements and remedies. Many supplements include herbs which are designed to help reduce inflammation and support the healing response.
My most recommended supplement to help recover from injury is Mt. Capra CapraFlex. Essentially, it combines an organic glucosamine and chondroitin supplement with other natural herbs which are designed to reduce inflammation and support healing. CapraFlex can be taken long term or intermittently.
Phenocane Natural Pain Management combines the following: Curcumin, an herb that reduces pain and inflammation; boswellia, a natural COX2 inhibitor that also reduces pain and inflammation; DLPA, an amino acid that helps to increase and uphold serotonin levels in the brain; and nattokinase, an enzyme that assists with blood clotting and reduces pain and inflammation.
Another supplement I frequently recommend to help recover from injury is Tissue Rejuvenator by Hammer Nutrition. It contains glucosamine and chondroitin as well as a host of herbs, spices, and enzymes to help support tissues and limit inflammation. It’s a fantastic supplement.
I recommend taking either CapraFlex OR Tissue Rejuvenator, not both concurrently.
I initially recommend trying a 30 day protocol. If the supplements are aiding your recovery, you may choose to continue taking them for an additional 30 days. I sometimes implement this protocol as part of a prevention strategy during times of heavy volume or high intensity training. (Please consult with your pharmacist and/or physician prior to starting any new supplementation protocol. Herbs could interact with some medications particularly if you are taking blood thinners.)
Improve your foot mobility and strength. Complete with instructions and photos, this guide, Morton’s Neuroma Rehabilitation Exercises, outlines how to safely perform exercises in order to improve your mobility and strength.
Weakness in the foot and ankle muscles (as well as the smaller foot intrinsic muscles) is often found in the case of Morton’s neuroma as part of the biomechanical issues that led to its development. I recommend initiating a complete ankle/foot strengthening protocol. Please refer to Ankle Resistance Exercises Using the Elastic Exercise Band.
Improve your balance. Poor balance is often associated with muscle weakness in the foot and ankle as well as the knee and hip musculature. Weakness and balance deficits can lead to poor foot biomechanics. Standing on one foot can be an excellent way to improve your balance. This technique is demonstrated in the Morton’s Neuroma Rehabilitation Exercises. For additional ideas on how to improve your balance, please refer to Improving Balance by Using a Water Noodle.
Research concludes that nearly 80% of all cases of Morton’s neuroma can be treated through conservative measures (as outlined above). In the rare cases where conservative measures fail, then one may need to consider surgical options.
One surgical option offered is decompression surgery. During this surgical intervention, the surgeon can relieve the pressure on the nerve by cutting nearby structures (such as the ligament that binds together some of the bones in the front of the foot). Unfortunately, this alters the shape of the foot and may affect foot dynamics into the future. Another option is to resect or remove the nerve. Surgical removal of the nerve is usually successful, but the procedure can result in permanent numbness in the affected toes.
If you’re not experiencing significant relief from Morton’s neuroma upon changing your footwear and addressing other risk factors while progressing into your exercise program, please consult a medical professional. I recommend a physical therapist that specializes in feet. The American Physical Therapy Association offers a wonderful resource to help find a physical therapist in your area.
Has a specific treatment for Morton’s neuroma helped you? Which treatments haven’t worked for you? Please leave your comments below.
Looking for that exercise or book I mentioned in a post? Forgot the name of a product or supplement that you’re interested in? It’s all listed in the Resource Guide. Check it out today!
If you have a question that you would like featured in an upcoming blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. Be sure to join our growing community on Facebook by liking The Physical Therapy Advisor!

Great read, Ben!
I never knew this specific pain had a name, I have to tell my sister who I think may have this. That test sounds so easy, that’s a great relief we can see at home for ourselves.
Do you know if it worsens if it goes untreated, or can it lead to any other issues?
I’ll be passing this post along!
Giuliana,
Thank you for the comment. A neuroma in the foot is relatively common. If left untreated, the pain tends to worsen over time which ultimately can affect how a person walks and his/her quality of life. People often tend to modify activities and compensate with abnormal gait patterns which can lead to other issues. Treatment is usually effective. I find most will need to at least temporarily modify his/her footwear. Definitely worth addressing in order to eliminate the pain and get back to normal activities.