Q. For the past several months, my 12 year old son has been experiencing pain below his knee cap just to the top of his shinbone. He typically experiences pain when playing soccer or other sports. The pain goes away when he rests. It’s getting to the point that it’s hard for him to participate in sports. He hasn’t had any injuries. What do you recommend? -Chandra
A. Thanks for your question, Chandra. I’m sorry to hear about your son’s knee pain. Unfortunately, it’s a common problem in children (particularly, boys). The symptoms that you are describing sound like Osgood-Schlatter disease although other potential causes could be Patellar Tendinitis or Patellar Femoral Pain Syndrome. Due to his age, gender, and activity level, it’s most likely Osgood-Schlatter disease.
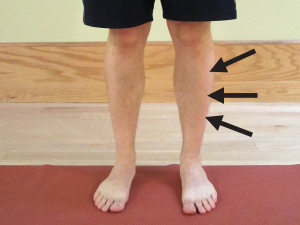
Osgood-Schlatter disease (OS) is an overuse injury with pain located just below the knee where the patellar tendon ends (inserts) on the Tibial tuberosity. A boney nob may start to develop in this area and usually occurs as the condition progresses. This occurs due to the excessive stress on the skeletal system during a period of rapid growing combined with stress from activity of the quadriceps muscle pulling on the patellar tendon at its insertion site on the bone. If a bump forms, don’t worry as it is benign with OS. It will likely continue to be there as your child ages. There are typically no long term effects for this condition except for pain over the raised area of bone when kneeling on a hard surface.

Risk Factors for Osgood-Schlatter disease include:
- Boys who are 11-13 years old.
- Period of rapid skeletal growth.
- Adolescents who regularly participate in running, jumping, and sports with many cutting or rapid changes in direction.
Symptoms for Osgood-Schlatter disease include:
- Pain and possible swelling below the knee located near the top of the shinbone.
- A bump or boney growth on the front of the upper shin at the Tibial tuberosity that is typically painful to touch.
- Pain with running, jumping, and cutting sports.
- Decreased pain or no pain at rest.
- Possible loss of knee range of motion, typically flexion.
- Possible pain and tightness with quadriceps stretching due to the pull on the patellar tendon.
- Loss of quadriceps strength which mostly due to pain inhibiting its use.
- Painful kneeling.
OS typically begins with mild soreness. The condition is typically self-limiting because of pain. Continuing to push through the pain can cause significant long-lasting pain resulting in limited function. Early intervention is usually very helpful.
My Top 5 Tips on How to Self-Treat Osgood-Schlatter Disease:
RICE
RICE, which stands for Rest, Ice, Compression, and Elevation.
Rest. In this case, rest would indicate tapering down from your regular exercise activity or any activity that involves running and jumping or that is causing knee pain.
Ice. Apply ice to the painful area–typically the sooner, the better. The rule for icing is to apply ice no more than twenty minutes per hour. Do not place the ice directly against the skin, especially if you are using a gel pack style. A bag of frozen peas can be ideal. Individuals with poor circulation or impaired sensation should take particular care when icing.
Compression helps to prevent and decrease swelling. Swelling can cause increased pain and slow the healing response, so limit it as much as possible. You can utilize a common ACE wrap. If you have a friend who is medically trained, many different taping techniques can also assist in decreasing swelling. You may also consider a compression sleeve or garment.
Elevation. If there is swelling, then elevating the leg may be helpful.
If it hurts, don’t do it!
Modify the activity or discontinue it completely. If your knee is hurting when performing your sport or activity whether you are running, jumping or even weight lifting, then discontinue the activity temporarily. If you are able to modify and perform the exercise or activity pain free, it would be okay to continue in most cases.
Improve your range of motion (ROM).
The primary goal of a rehabilitation program is to regain full pain free ROM for knee flexion (bending) and extension (straightening). This can be accomplished in many ways. Perform heel slides by lying on your back and sliding your heel toward your buttocks. Consider using a pole to assist in performing deeps squats. Another stretch would be to hang onto a pole or a doorframe, and bring your heel toward your buttocks as you perform a quadriceps stretch.
These exercises should only be performed within a mild to moderate amount of discomfort in order to regain full pain free ROM. If you experience muscle tightness and soreness, I recommend using a foam roller to assist with any myofascial symptoms. To learn how to use a foam roller, please refer to Foam Rolling for Rehabilitation.
Work on strengthening.
The primary goal of a strengthening program is to work on the quadriceps and glutes medius (hip abduction). Weight lifting is an appropriate choice, but you may have to initially limit your range of motion (ROM). Most of my clients begin on a non-weight bearing program, then progress to partial weight bearing, and eventually, full weight bearing. The more severe the symptoms, the longer it will take for an individual to progress to more difficult exercises or to increase the resistance (load).
To initiate a physical therapy program, please refer to Osgood-Schlatter Disease Rehabilitation Exercises. This exercise guide is designed to address the muscles that I find to be the weakest in most individuals. The exercises are listed from easiest to most challenging and are designed to primarily improve quadriceps and hip strengthening. Initially, focus on full ROM.
Weight training exercises (with machine weights or free weights) should be geared toward general leg strengthening and may include: squats; leg press; hip abduction machine; step ups; dead lifts; and straight leg dead lifts. If further instruction is needed, search YouTube to watch the proper technique for a specific exercise. Do not perform any seated knee extension exercises.
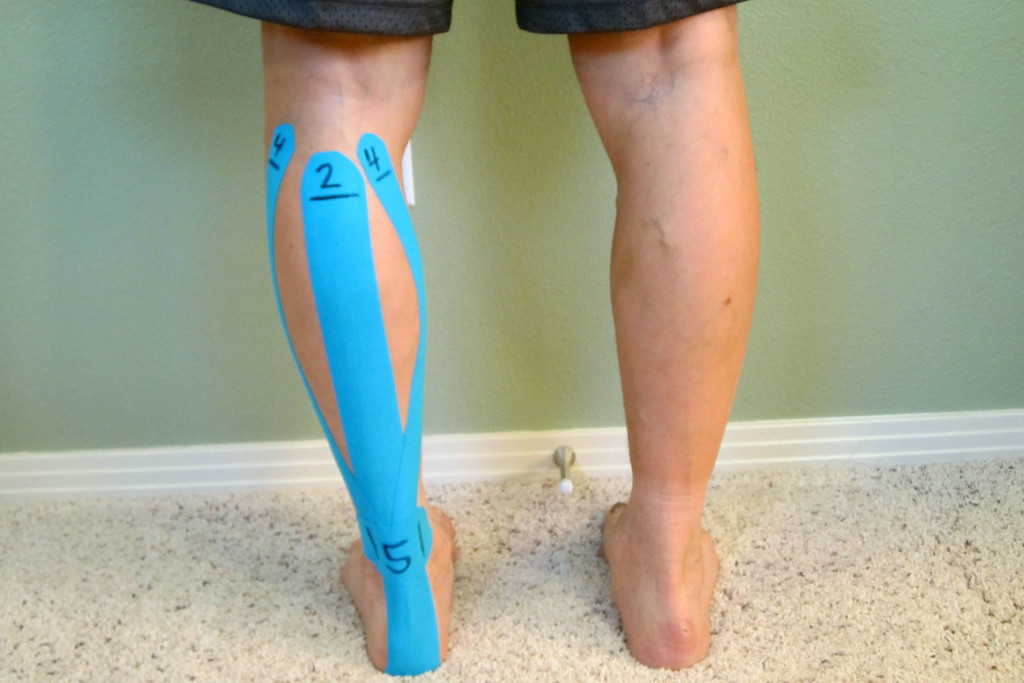
Kinesiological taping.
Besides pain relief, the purpose of Kinesiological tape is to provide compression over the Tibial tuberosity and to facilitate additional blood flow to the area. It also provides proprioceptive input which can help the knee during activity. I have had luck using Kinesio Tape, Rock Tape, and Mummy Tape brands. There are many other useful taping techniques which utilize different forms of tape. (You could also utilize Spider tape or KT TAPE.) To visually learn how to apply the tape, please refer to Kinesiological Taping for Osgood-Schlatter Disease. For application and removal tips, please refer to Skin Care with Taping.
How to Prevent Osgood-Schlatter Disease:
Be sure to schedule rest between athletic seasons, athletic events, and higher volume training periods. Rest is a critical factor as an adolescent’s body undergoes physical changes. OS is typically associated with overtraining/overuse in combination with a rapidly growing skeletal system. There are times when an adolescent needs to rest. It’s important not to encourage an adolescent to play sports through the pain without adequate recovery, rest, and if necessary, an evaluation by a qualified physical therapist or physician.
As part of a prevention and cross training strategy, implement the exercises demonstrated in the Osgood-Schlatter Disease Rehabilitation Exercises. A proper warm up and cool down is critical when performing in an athletic event or a significant training session.
- Warm up prior to exercise. I recommend that you increase your normal warm up time by at least 10 minutes in order to increase blood flow to the area. This allows better mobility and also promotes healing as movement is necessary to bring in the nutrients. Use a stationary bike or the rower machine initially to get the muscles warm and the knee joint more lubricated. Then work on moving into a deep squat position multiple times as part of the warm up. You may need to hang onto a beam or a pole to take some pressure off of your knee as you move in and out of the squat.
- Cool down. After performing your exercises, take extra time to cool down and stretch. Use either a stationary bike (at a causal/slower pace) or the rower machine. Both are reduced weight bearing exercises that promote movement and circulation to the knee as well as increasing ROM. This is the perfect time to work through my recommended rehabilitation exercises.
Thank you, Chandra, for your question! I hope these tips will help you assist your son in his recovery and get him back to playing sports as quickly as he is able to without pain! If the pain continues, please seek additional assistance from a qualified physical therapist or physician. The American Physical Therapy Association offers a wonderful resource to help find a physical therapist in your area.
Do you know an adolescent who may be suffering from Osgood-Schlatter disease? If so, please share my recommendations on how to address this common and treatable condition.
If you have a question that you would like featured in an upcoming blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. Be sure to join our growing community on Facebook by liking The Physical Therapy Advisor!
Disclaimer: The Physical Therapy Advisor blog is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice. No health care provider/patient relationship is formed. The use of information on this blog or materials linked from this blog is at your own risk. The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Do not disregard, or delay in obtaining, medical advice for any medical condition you may have. Please seek the assistance of your health care professionals for any such conditions.