Q. My hand grip has been feeling weak, and I have noticed some tingling in my first two fingers. Do I have Carpal Tunnel Syndrome? I use my hands all day long, and I can’t miss work for surgery. Is there anything I can do? -Jared
A. Thanks, Jared, for the great question! Carpal Tunnel Syndrome (CTS) is a very common cause of hand pain and weakness. It’s also often associated with numbness and tingling particularly in the thumb and first (index) and second (middle) finger. It’s often accompanied with associated motor control issues within these fingers. The symptoms tend to start gradually and typically worsen over time. The pain can get to a point that is unbearable. One can lose functional use of their hands because of the pain, numbness, and associated lack of motor control.
Symptoms of Carpal Tunnel Syndrome:
- Pain in the wrist, palm of your hand, and/or fingers.
- Numbness and tingling in the thumb and first (index) and second (middle) finger. The median nerve is affected. The fourth (ring) finger and pinky finger are not directly affected because it’s a different nerve (ulnar). Along with numbness and tingling, many people will describe an electric shock type feeling in these same fingers. Initially, the numbness and tingling is intermittent, but it can progress into a constant sensation.
- People describe the lack of hand control and the tendency to drop objects.
Symptoms tend to worsen when gripping or performing hard manual labor, including repetitive motions with the hands that involve flexion (closing) of the hand. Symptoms are often worse at night and may even wake you up.
Causes and Risk Factors for Carpal Tunnel Syndrome:
- Pressure over the median nerve near the palm of the hand in the “Carpal Tunnel” which is a type of passageway from your forearm to your wrist.
- Repetitive motion. CTS is typically viewed as a repetitive motion or overuse injury. Repetitive gripping and heavy use of the hands can lead to irritation of the median nerve. This means that professions involving heavy use or repetitive use of hands (particularly, if there is vibration) are at higher risk of developing CTS. This can range from manual laborers to pianists or typists.
- Scar tissue build up and/or fascial restrictions in or around the carpal tunnel from repetitive use or trauma such as repeated compression. Chronic vibration of the hands and arms is a risk factor. Examples include heavy use of power tools (such as a jack hammer) or motocross racing.
- A wrist fracture can narrow the tunnel space from swelling and inflammation or cause deformation of the bones in the wrist.
- Swelling and inflammation from other pathologies such as Rheumatoid arthritis or cysts.
- Any injury or pathology that causes deformation of the bones in the wrist that places additional pressure on the median nerve. This would include obesity as fat deposits can reduce the space within the carpal tunnel.
- Females are more likely than men to develop CTS. This is likely due to anatomical variations where the carpal tunnel is typically smaller in women versus men. This allows the area to be more easily compromised or affected from other causes.
- Fluid retention may increase the pressure within your carpal tunnel and be irritating the median nerve. This is common during pregnancy and menopause. CTS associated with pregnancy will typically resolve on its own after pregnancy.
- Muscle imbalances between wrist flexion and extension strength.
- Mobility related issues in the wrist, shoulder, thoracic, and cervical spine.
CTS can be straightforward with a very typical mechanism of injury or can be very difficult to treat because of multiple factors leading to the syndrome. Often it’s a multitude of risk factors that cause the symptoms in addition to anatomical variations from person to person. Other compounding factors include: diabetes; thyroid disease; kidney failure; other forms of inflammatory arthritis; poor posture; and cervical and thoracic derangements.
Poor wrist, shoulder, cervical, and/or thoracic mobility is often associated with CTS and other spine and/or upper extremity pain syndromes. I find that even in the clearest cut of cases it’s always best to screen for other potential causative factors by starting with the cervical spine and working down the chain into the hand. Whenever one part of the body doesn’t have adequate mobility, another part will do more to allow for the movement to take place.
My Top Recommendations to Alleviate Pain associated with Carpal Tunnel Syndrome:
Identify the offending movement.
If you’re experiencing CTS pain, try to identify which specific movement aggravates the symptoms. Once you identify the movement, find ways to either avoid the motion or to change how you perform the activity as to not cause the symptoms. This may mean adjusting your posture or body position or using an adaptive device to help your body compensate for the activity. Eliminate as many of the noted risk factors from your daily activities as you can.
Work on your grip strength through extension movements.
Don’t just work on wrist flexion or gripping exercises. Also work on finger and wrist extension in order to improve your grip strength. Often in the case of CTS, there is a muscle imbalance between your ability to flex your fingers and wrist versus extending your fingers or wrist. Work on extension biased exercises. Your grip strength will improve more rapidly as your wrist and hand muscles find their optimal length tension relationship (which allows for maximum strength production).
For wrist extension, use an exercise band (as demonstrated below) to perform two to three sets of 20 repetitions. Extend the wrist up, and then slowly back down toward the floor. Be sure to move very slowly during the eccentric/muscle lengthening position (when your hand returns to the floor).

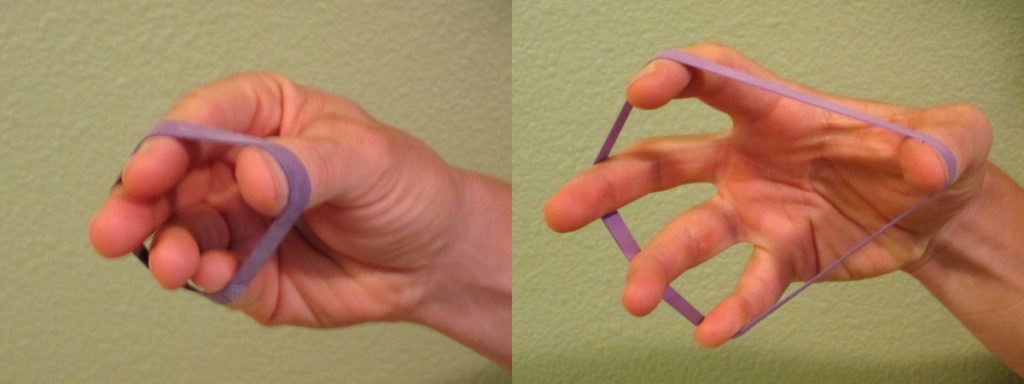
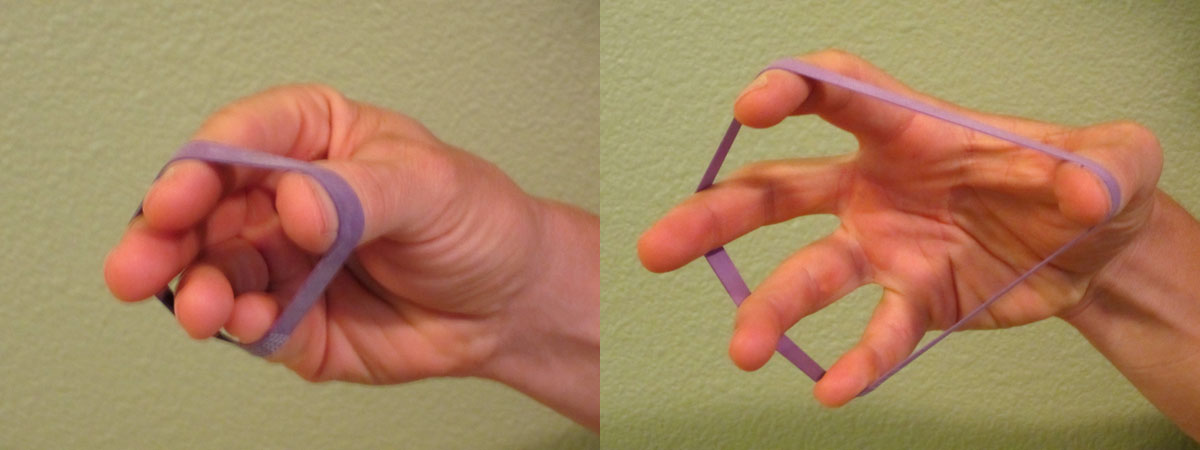
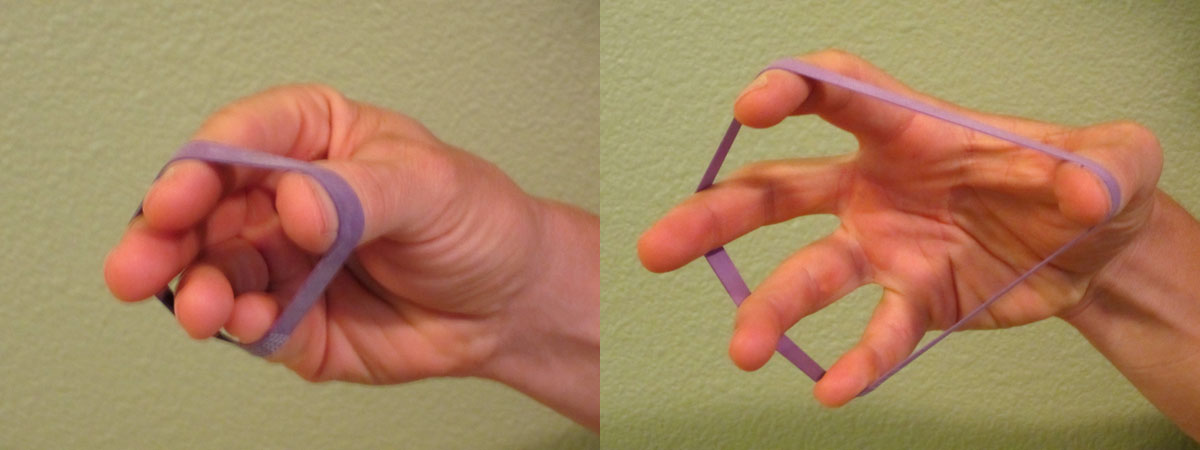
To improve finger extension strength, I often recommend using a thick rubber band as a way to improve finger extension strength (as demonstrated below). Work on extending each finger equally when performing two sets of 10-15 repetitions multiple times per week.
If you want to be more precise and have the ability to exercise one finger at a time, try a device such as the CanDo® Digi-Extend® Hand Exerciser. This is an excellent tool to improve finger extension strength. It allows you to work the fingers in multiple ways including individually for rehabilitation purposes and as an important hack to improve overall grip strength (as described above). It also allows for customization of resistance so you can track progress.

Stretch.
I suggest stretching the fingers and wrist multiple times a day. Your fingers and wrist should have mobility in all directions. Particularly focus on wrist extension (as demonstrated below). Perform two to three sets of a 30 second stretch three to five times per day as long as you do not reproduce your CTS symptoms.


Work on your mobility.
Restrictions in mobility typically don’t just occur in the fingers and wrist, but also up the arm and into the thoracic and cervical spine. I like to use items, such a PVC pipe, that you might already have at home. This works great for forearm mobilization. You could also use a golf ball. You can use one hand to press or rub the PVC pipe over sore or tender areas. The amount of pressure shouldn’t be painful. Avoid pressing on especially boney areas.

Poor mobility elsewhere in the kinetic chain can and will affect hand and wrist symptoms. Work on upper body mobility by focusing on shoulder and thoracic mobility. You can automatically download my FREE resource for shoulder and thoracic mobility, My Top 8 Stretches to Eliminate Neck, Upper Back, and Shoulder Pain, when you subscribe to my e-mail list.
Be proactive.
Once you start to feel pain, be aggressive with your management and self-treatment. Implement these recommended exercises, stretches, and mobilizations quickly so you can stop the pain from progressing. It’s always easier to intervene early. Take your rehabilitation seriously and perform the exercises diligently while you work to eliminate risk factors that may be affecting the condition.
Contact your Physical Therapist (PT).
If the pain persists, seek additional help. Don’t let the pain linger. The longer it’s left untreated, the more potential for harm and damage (which potentially could lead to a longer recovery). The American Physical Therapy Association (APTA) is an excellent resource for learning more about physical therapy as well as locating a physical therapist in your area.
Thanks for the question, Jared! Carpal Tunnel Syndrome (CTS) can be debilitating by limiting your ability to exercise, work, and perform daily tasks. Be proactive in your care and management. Most importantly, don’t let the pain and symptoms linger. The longer you have the symptoms, the harder they can be to eliminate and recuperate from.
Have you ever dealt with Carpal Tunnel Syndrome (CTS) pain? Which treatments have you found to be the most effective? Additional discussion can help others to manage their pain. Please leave your comments below.
If you have a question that you would like featured in an upcoming blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. Be sure to join our growing community on Facebook by liking The Physical Therapy Advisor!