Q. Hi, Dr. Ben. I was recently diagnosed with moderate COPD. I “knew” I have had it for a few years, but I didn’t want to admit it. What exercises do you recommend that I perform to keep my lungs functioning at their best capacity? I know I need to keep active, keep a healthy lifestyle, and keep going! I gave up smoking last week when I was diagnosed. I am not on oxygen at this time. Inhalers are being used to manage my COPD at this time. I hope this will help others from being stubborn, choose to give up the smokes, and “get real” because this can happen to any of us! Thanks, Ben! -Linda
A. Thanks for your question, Linda! I am sorry to hear about your recent diagnosis of COPD. It sounds like you are already making some appropriate and much needed lifestyle changes to help to manage the disease.
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease (meaning it worsens over time). COPD is currently the third leading cause of death in the United States. It is typically diagnosed in middle aged or older adults. Cigarette smoking is the leading cause of COPD. Most cases of COPD are associated with those that have smoked, used to smoke or who were around heavy amounts of smoke. Other potential causes include: exposure to chemicals that irritate the lungs (such as air pollution, chemical fumes from paint or other industrial causes); exposure to high levels of dust and dirt; and genetic factors.
Symptoms of COPD:
- Coughing (typically producing large amounts of mucus).
- Wheezing.
- Shortness of breath (SOB).
- Tightness in the chest.
With COPD, there is less air flow in and out of the lungs. This can occur for one or several of the following reasons:
- The airways and air sacs (alveoli) lose their elasticity.
- Walls between the air sacs are damaged and/or destroyed.
- Ways of the air sacks become thick and/or inflamed.
- There is excessive mucus production in the air sacks causing them to clog.
COPD is most commonly associated with two conditions, either emphysema or chronic bronchitis. In the case of emphysema, the walls of the air sacs are damaged and/or destroyed which leads to less air sacks (alveoli) to assist in gas exchange during breathing. In the case of chronic bronchitis, the lining of the airways is chronically irritated and inflamed. This leads to a thickening and excessive mucus production, which blocks the airways and causes difficulty with breathing. Generally individuals with COPD tend to have both emphysema and chronic bronchitis.
Those with COPD are especially prone to other illnesses, such as colds, flu, and pneumonia, and they are in a high risk category. Although controversial in western medicine, I am convinced that proper supplementation of key nutrients can assist your immune system in fighting many common illnesses.
Strategies for managing COPD:
Medication.
Your physician will likely prescribe medications to help you to manage COPD. These will typically include anti-inflammatory medications and bronchial dilator medications. Be sure to always follow your physician’s advice when utilizing prescription medication.
Stop smoking.
This may sound obvious, but smoking cessation is critical to managing COPD. Smoking was likely a major contributing factor to developing COPD. It will be very difficult to manage the disease long term if you do not stop smoking. If a person continues to smoke, lung function and prognosis for disease management will decline at a much faster rate than average. Many programs are available that can help you to quit smoking. Please speak with your physician to learn more about resources in your area.
Daily activity.
Daily activity is important for everyone, but especially for those with COPD. A sedentary lifestyle will only worsen your symptoms. Depending on the severity of your COPD, your ability to perform certain activities will vary. For more information, please refer to How to Jumpstart a Sedentary Lifestyle and Why You Should Walk, Not Run.
As your disease progresses, it will become increasingly difficult to remain active. Activity modification will be part of your management strategy, but continue to do what you can. It is critical to keep regular activity as part of your disease management strategy.
Exercise.
It is critically important that you engage in specific, purposeful exercise. A thorough exercise program should include components of each of the following:
- Weight Training
- Cardiovascular Exercise
- High Intensity Training
Each exercise program should be specifically designed for the individual. These three forms of exercise have significant research in improving physical function (including muscular, cardiovascular, and pulmonary function). It is extremely important that your exercise program is properly dosed and prescribed just for you. As your disease progresses, your dosing and exercise prescription will also change. To adequately mange the condition, you must implement a thorough exercise program.
You will likely need assistance in designing a program specifically for your needs. First, please speak with your physician. Then seek a qualified physical therapist that specializes in cardiovascular disorders. The American Physical Therapy Association offers a wonderful resource to help find a physical therapist in your area. In most states, you can seek physical therapy advice without a medical doctor’s referral (although it may be a good idea to seek your physician’s opinion as well). Another option is to seek a local cardiac and pulmonary rehabilitation program in your area. These are usually associated with your local hospital.
As your disease progresses, it will become increasingly difficult to exercise, but continue to do what you can. The intensity and duration may change and you will need additional rest. It is critical to maintain some form of exercise as part of your disease management strategy. This is an exercise is medicine approach.
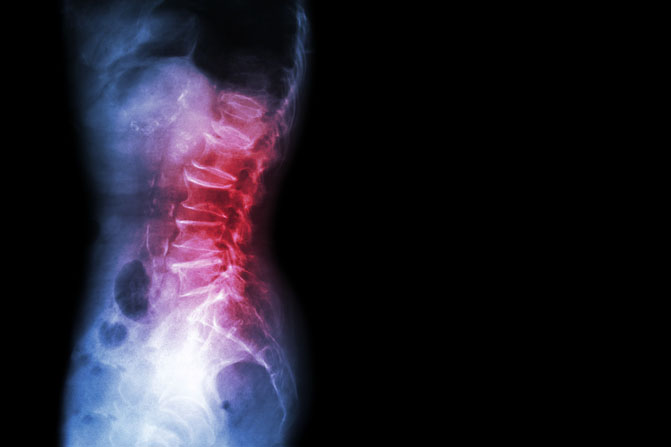
Rib and thoracic mobility.
Addressing rib and thoracic mobility is one way to make quick improvements in a person’s ability to breathe and generally improve endurance and lung function. Unfortunately, this is underutilized in most COPD sufferers.
Since COPD affects the lungs, restrictions in the musculature and the skeletal system that encase the lungs will only worsen a person’s breathing difficulties. The key is to help your body move as efficiently as possible. In order to achieve this, the ribs and thoracic spine along with the associated musculature must be free to move. Any restrictions in this area will only make it more difficult to breathe.
When you sign up to receive my blog posts via e-mail, you will automatically gain access to my FREE resource, My Top 8 Stretches to Eliminate Neck, Upper Back, and Shoulder Pain. These exercises address the most common rib and thoracic restrictions, so that you can maximize your rib and thoracic mobility in order to breathe easier. Detailed photos and exercise instructions will help you to get started. I recommend that you combine these with a daily deep breathing program.
Deep breathing.
Learning a variety of breathing techniques will also be a critical component in managing COPD. Deep breathing allows the body to uptake more oxygen. It also helps to reduce stress and anxiety. The mechanical act of breathing more deeply helps your ribs and thoracic spine to remain mobile. It also helps to train all of the muscles associated with breathing–from the diaphragm and intercostal muscles to the lesser known accessory breathing muscles (sternocleidomastoid, the scalenes, serratus anterior, pectoralis major and minor, trapezius, latissimus dorsi, erector spinae, iliocostalis lumborum, quadratus lumborum, serratus posterior superior and inferior, levatores costarum, transversus thoracis, and the subclavius).

When performed properly, deep breathing can help you to maintain your lung capacity. An incentive spirometer should be used regularly as part of maintaining proper lung capacity and function. It can also decrease your risk of pneumonia, which is always a concern for those with COPD.
Learning multiple methods of breathing will be important as you progress in your disease management. Each method is used for a different situation. Along with deep breathing exercises, diaphragmatic and pursed lip breathing techniques will also be beneficial.
Adequate sleep.
Poor sleep is linked to the following cardiovascular risk factors: high blood pressure; atherosclerosis; heart failure; heart attack; stroke; diabetes; and obesity. These all have negative effects on COPD management.
Be sure to get as much sleep as you need (typically 7-9 hours at night). Short naps are also an excellent way to get more sleep. I recommend that you read Michael Hyatt’s 6 Strategies to Sleep Soundly, Wake Rested, and Accomplish More.
Acupuncture is also a proven method to help people sleep better and more soundly. It can be used to treat insomnia as well.
Reduce your stress.
Stress is a normal part of life. Poorly managed stress or excessive stress can lead to emotional, psychological, and physical problems, such as cardiovascular disease and high blood pressure. High stress leads to more anxiety which can affect breathing patterns. Individuals with COPD will already struggle at times with breathing, which will worsen as the disease progresses. High stress will only make this worse. Regular exercise, massage, yoga, acupuncture, and Tai Chi have all been proven to reduce stress.
Maintain a healthy weight.
Additional weight makes it more difficult to move around. It also creates additional pressure in the rib cage–making breathing more difficult. The heavier you are, the more difficult it will be to exercise which is a critical component of COPD management. Obesity is associated with diabetes, high blood pressure, and coronary artery disease. These all increase your risk of developing heart disease and have a negative effect on health and COPD management. Studies have shown that excess body weight (not including all of the other associated medical conditions) can also lead to heart failure. Even if you are healthy otherwise, being overweight still places you at a greater risk of developing cardiovascular and pulmonary related diseases.
Stay hydrated.
Drink more water. The older you are, the easier it is to become dehydrated. Proper hydration is critical to keeping lung tissue healthy. The human body is primarily made of water, which is critical for all body functions. Dehydrated tissues are prone to injury as they struggle to gain needed nutrients to heal and repair. Dehydrated tissues are less flexible and tend to accumulate waste products. Water intake supports proper brain, lung, muscle, and hormone function as well as lubrication of the joints and skin appearance.
Stay hydrated by drinking water. Try to avoid beverages that contain artificial sweeteners or chemicals with names that you can’t spell or pronounce. Drinking more water not only prevents dehydration, but it also aids in preventing urinary tract infections (UTI).
Living with and managing COPD will be a different journey for everyone. When managed correctly, individuals with COPD can live a long time. Although there isn’t presently a cure for COPD, treatment options continue to improve every year. The important part is to start addressing the disease early through medication management and lifestyle changes including: smoking cessation; healthy eating and proper hydration; stress management; breathing techniques; and optimizing your exercise and activity levels in order to maintain proper rib and thoracic mobility.
Thanks for your question, Linda! For additional information on the topic of COPD, please visit the following: http://www.nhlbi.nih.gov/health/health-topics/topics/copd/ and http://copd.about.com/od/copdbasics/a/copdlifeexpectancy.htm.
Do you or a loved one suffer from COPD? Please share your experience with us. Together we can all grow and learn how to best manage this disease.
If you have a question that you would like featured in an upcoming blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. Be sure to join our growing community on Facebook by liking The Physical Therapy Advisor!
Disclaimer: The Physical Therapy Advisor blog is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice. No health care provider/patient relationship is formed. The use of information on this blog or materials linked from this blog is at your own risk. The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Do not disregard, or delay in obtaining, medical advice for any medical condition you may have. Please seek the assistance of your health care professionals for any such conditions.